Oral Health, Pregnancy, and Tobacco Use: Dr. Chintan Desai on Community Myths and Real Risks (Part-4)
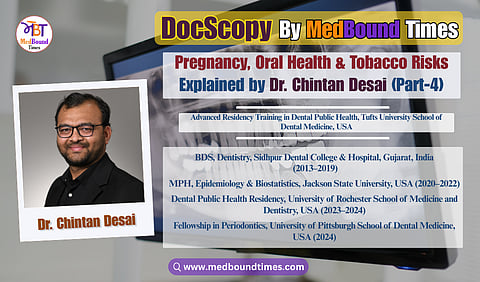
In this edition of MedBound Times, Himani Negi and Dr. Akriti Mishra speak with Dr. Chintan Desai, a Dental Public Health professional currently pursuing advanced residency training in Dental Public Health at the Tufts University School of Dental Medicine. With a strong foundation in clinical dentistry and a growing focus on population health, Dr. Desai represents a new generation of dentist–public health leaders working at the intersection of care delivery, research, and health equity.
A BDS graduate from Sidhpur Dental College, Gujarat, and holder of a Master of Public Health in Epidemiology and Biostatistics from Jackson State University, Dr. Desai has trained at renowned institutions including the University of Pittsburgh School of Dental Medicine and the Eastman Institute for Oral Health, University of Rochester. His work on NIH-funded projects and large public health initiatives has strengthened his expertise in data-driven research, program evaluation, and evidence-based dentistry.
Dr. Desai’s academic interests span oral–systemic health, periodontal disease, and epidemiological research using national health databases. He has co-authored peer-reviewed publications in journals such as Cureus and the Journal of Perinatology, presented at forums including AADOCR, NOHC, and the New York State Oral Health Summit, and serves as a peer reviewer for international dental and biomedical journals.
Beyond research, he is deeply committed to preventive care and health equity, contributing to school-based oral health programs, maternal and child initiatives, and community outreach addressing early childhood caries and access to care. His dedication to ethical, service-oriented dentistry has earned him selection as a Fellow of the International Pierre Fauchard Academy (India Section).
In the Part 4 of this interview series at MedBound Times, conducted by Himani Negi and Dr. Akriti Mishra, Dr. Chintan Desai addresses common myths surrounding dental care during pregnancy, explains the link between oral and systemic health, and reflects on community challenges in tobacco cessation and oral cancer awareness.
Himani Negi: I would like you to address a common myth. During my training, I observed that many pregnant women avoid going to the doctor for minor pains or other issues. This often stems from the misconception that taking any medication could harm their child. I seek to clarify this issue: if they are experiencing problems, whether related to dental health or other concerns, what steps should they take?
Dr. Chintan Desai: This is a common misconception. Some medications are unsafe during pregnancy, but many dental treatments and commonly prescribed medications are completely safe when used correctly. What is more harmful is ignoring dental pain or infection because untreated disease can create greater risk for both the mother and the child.
We follow clear guidelines. For example, drugs like Tetracycline are avoided because they can affect the developing teeth of the child, but safe alternatives such as Amoxicillin and Penicillin are available. The same applies to dental X rays. We do not avoid them completely. They can be taken safely when needed, with proper shielding, and we simply avoid unnecessary imaging.
Pregnant women should visit the dentist regularly because hormonal changes increase the risk of gum problems. In clinics we also take precautions such as keeping appointments short and ensuring comfortable positioning. The most important message is that dental care during pregnancy is both safe and necessary. Patients should not delay treatment. They should consult a trained provider who can offer the right medication and the safest approach for their situation.
So, we can conclude that instead of relying on pharmacy advice, pregnant women should go to a doctor and find out what is suitable for them, instead of just assuming and taking careless action, I would say. Pharmacists are knowledgeable, but they do not evaluate the full medical history or the stage of pregnancy, which are essential for deciding whether a medication is safe. Some drugs, like ibuprofen in the later stages of pregnancy, should be avoided, while others, like acetaminophen, are usually safe when used appropriately. These decisions require clinical judgment.
Doctors and dentists follow established guidelines for caring for pregnant patients, so they can provide treatment that protects both the mother and the baby. The message is simple. Pregnant women should not self medicate. They should speak with a doctor or visit a clinic whenever they have a dental or medical concern.
Dr. Akriti: We now see that lifestyle diseases, like diabetes and obesity, are very prevalent. How does this impact oral health? How do you explain to the general public that if they are having some health issue, it might have an impact, given that uneducated people don't know the connection?
Dr. Chintan Desai: That is a very important question, because many people do not realize how closely lifestyle diseases and oral health are connected. When we speak with the general public, especially in communities with limited health knowledge, verbal explanations alone are not enough. Most people understand better when they can see something in front of them.
During outreach programs, we use simple tools like pictures, charts, short videos, and brochures. For example, when we talk about obesity, we show how weight and height relate to each other through a basic chart. Once people see their body mass index category, it becomes easier to explain the possible health risks, such as the increased chance of developing Type 2 diabetes. After that, we connect it to oral health by explaining how diabetes can affect the gums, slow healing, and increase the risk of infections in the mouth.
We also give one page brochures that describe these connections in simple language and list the steps they can take to protect their health. These handouts help them remember the information and share it with their families.
Another effective method is using short educational videos. We create a link or a barcode that people can scan. They can watch the information immediately or when they return home. This makes learning easier and more comfortable for them.
When we use visual and practical methods, people begin to understand that oral health is part of their overall health. Seeing the information has a stronger impact than hearing it, and it encourages them to make small changes that can improve their health in the long run.
Basically, the main goal is to make the information relatable and easy for them to understand. As healthcare professionals, we are trained to think in medical terms, but our patients are not. So we should always try to see the message from their point of view. When we keep their background, language, and daily challenges in mind, the information becomes much clearer for them. Our role is to simplify, not complicate, and to make their learning experience as comfortable as possible.
Dr. Akriti: This question focuses on oral cancer and the community's response to oral health education regarding it. In India, statistics show that in some states, children begin using tobacco at a very young age. This situation often arises from community norms, a lack of proper knowledge, insufficient parental guidance, or peer encouragement. As a result, many children start abusing substances early in life and face long-term consequences.
When we engage with these communities and inform them about the negative health impacts of tobacco use, what questions do they typically ask in response? How do we educate them? Since smoking is often a deeply ingrained habit, simply telling individuals to stop is usually ineffective. If someone has just begun smoking or using tobacco, they are unlikely to notice immediate adverse effects, as it takes years for the consequences to manifest.
So, what strategies can we employ to help them break this habit? How do we motivate individuals to change their behavior?
Dr. Chintan Desai: Thank you for the question. I appreciate you asking that question. When we talk about oral cancer in the community, especially in areas where tobacco use begins at a young age, the response is mixed. Many people grow up in an environment where chewing tobacco or smoking is common, so they do not always see it as a danger. Some listen carefully, while others are not ready to accept the message because it has become a part of their daily routine.
In my outreach work, the most effective approach has been to make the education visual and practical. If I only give a verbal warning, people may not pay attention. But when they see pictures of early and advanced oral cancer or examples of how tobacco limits the ability to open the mouth, the message becomes real. We also use simple demonstrations that help people understand what tobacco does to the body. For example, in many awareness programs, we show how smoke collects in a sponge and then squeeze it out to reveal the dark residue. This is not a clinical test, but it is a powerful visual that helps people understand the harmful effect of smoke.
The questions we receive depend on the person. Some will not ask anything because they do not plan to change. But many people who are interested ask thoughtful questions. They want to know the side effects, the long term risks, and the early warning signs. I explain that a normal ulcer should heal within a week. If an ulcer does not heal in seven to ten days, or if there is a white or red patch that does not go away, they should seek screening or a biopsy. These early signs are important for catching the disease in time.
We also discuss the challenges of quitting. People often say they cannot stop because they have used tobacco for many years. In India, support to quit varies from place to place, and many people do not know where to get help. In the United States, there is more structure. People can call a quit line, and counselors guide them step by step. They explain the process, give advice, and follow up to support the person through the change.
Overall, the most effective strategy is patience, visual education, and clear guidance. People may not stop the habit immediately, but when we communicate in a way they can understand and relate to, we begin the process of change.
While addressing myths and misconceptions is essential to changing oral health behaviors, awareness alone is not enough. In part 5, Dr. Chintan Desai moves from belief systems to real-world action, sharing on-ground experiences that reveal how effective outreach programs, mobile clinics, and sustained community engagement can translate awareness into measurable oral health impact.