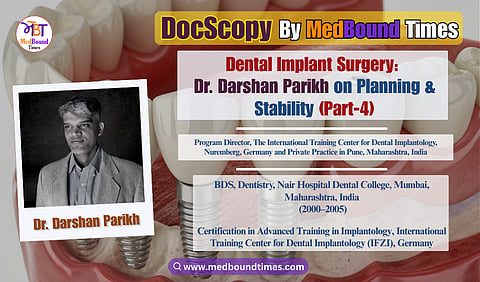
Implant Surgery in Practice: Dr. Darshan Parikh on Planning, Complications, and Clinical Judgment (Part-4)
In this edition of MedBound Times, Himani Negi and Dr. Akriti Mishra speak with Dr. Darshan Parikh, a general dentist skilled in oral implantology. Dr. Darshan Parikh, a graduate of the prestigious Nair Dental College, Mumbai. He maintains a curated boutique practice in the heart of Pune City. A Certified Mastercourse Instructor for the International Training Centre for Dental Implantology, Germany. He is currently the Program Director for IFZI in India, and trains dentists in practical Implantology. A regular marathon runner and sports enthusiast, he believes that correct training is what it takes to get across the finish line.
In the part 4 of this interview series at MedBound Times, conducted by Himani Negi and Dr. Akriti Mishra, Dr. Darshan Parikh brings focus to the surgical nuances involved in implant dentistry. He shares practical insights that come from real-world experience rather than textbook protocols.
Dr. Akriti: What are the key steps or precautions that you take to ensure that there is high primary stability and a good osseointegration in future?
Dr. Darshan Parikh: This ties directly into the importance of initial planning and diagnosis, which is absolutely critical in implant dentistry. Learning how to diagnose correctly, and more importantly how to interpret a CBCT accurately, is a key skill. Before any implant surgery, a significant amount of mental and technical planning happens. Personally, I spend at least 15–20 minutes before surgery running through the entire plan in my head. This includes confirming the implant diameter and length I intend to place, as well as identifying backup options. For example, if I have planned a particular implant size, I will always be prepared with an alternative diameter or length in case the clinical reality differs from what the scan suggests. At times, ridge width may appear adequate on the scan but turn out to be narrower once the flap is reflected. The sinus may be closer than anticipated, or bone height may be less than what the report indicates. Being mentally prepared for these possibilities is something that should happen multiple times, well before the flap is ever raised. Typically, once the scan report is available, I make written notes and often revisit the plan a couple of times. On one review, I may decide on a 4 × 8 mm implant; on another, after reassessing the anatomy, I may feel a 4 × 10 mm implant is possible, or I may decide that graft material should be kept ready if the sinus is close. This repeated review sharpens decision-making and reduces intraoperative surprises, in case of conventional workflow. When digital workflows are available, planning becomes even more robust. With access to planning software and raw DICOM data, the CBCT scan can be viewed three-dimensionally. For complex cases, I often sit with my lab technician and virtually place implants using planning software. This allows us to assess implant positioning, prosthetic alignment, and proximity to anatomical structures in detail. The one parameter that still remains difficult to judge digitally is bone density, which ultimately becomes a clinical judgment during surgery.
This is why a thorough understanding of your implant system is essential. It is not enough to know how to place an implant, you must understand how that specific system works: drill sequences, RPMs, the concept of osteotomy under-sizing, and how to modify protocols based on bone quality. Following the manufacturer’s guidelines is non-negotiable, especially in the early stages of your learning days. Understanding the limitations or the design parameters of the implant that you have chosen for that particular case are also important.
Once surgery begins, tactile feedback becomes invaluable. You start developing a “feel” for the bone. In cases involving multiple sites or quadrants, this feedback can directly influence how you modify your approach. For example, once during a full-mouth case, we encountered very soft bone in one quadrant of the maxilla, resulting in lower primary stability. When operating on the contralateral quadrant later, we deliberately undersized the osteotomy to improve stability. This ability to adapt comes from being receptive to feedback, both from the bone and from prior experience.
Primary stability is especially important if immediate loading is planned. If adequate stability is not achieved, the implant can still be placed and submerged, allowing a longer healing period before loading. There is no single rigid protocol; implant dentistry requires flexibility, sound judgment, and respect for biological principles.
From an objective assessment standpoint, tools such as resonance frequency analysis devices (Osstell or Penguin) can be used to measure implant stability. These provide numerical values that correlate with bone–implant contact and the degree of osseointegration. While not mandatory in every case, they offer valuable feedback and add an evidence-based dimension to clinical decision-making.
Finally, the learning curve in implant dentistry never truly ends. Continuous education is essential. Attending conferences, seminars, and lectures allows you to constantly refine your knowledge base and adapt to new clinical challenges. The goal is not just to place implants, but to place them predictably, safely, and in a manner that serves the patient well over the long term.
Dr. Akriti: Can you share some common complications that you have encountered in your practice so far, and how did you manage them?
Dr. Darshan Parikh: In the early phase of my practice, this was very much my experience. You begin working on a patient, and once you start reflecting the flap, you encounter bleeding. If the flap reflection is not adequate, the bleeding increases further, and visualization of the bone becomes compromised. At that stage, you are essentially working with limited visibility, almost blindly. This directly affects confidence. Until you build that confidence and your surgical steps start flowing smoothly, it takes time for your surgical acumen to develop. The second major challenge arises from inadequate case selection, particularly when the scan has not been read properly. In the initial phase, let us say the first two, three, or even four dozen cases, it is essential to choose cases with good bone volume. Borderline or doubtful cases should never be attempted independently at that stage. Such cases should always be done with a senior colleague, a mentor, or with a consultant actively involved in the surgery, so that you can observe how they manage unexpected situations intraoperatively.
While we have not had catastrophic experiences, it is important to acknowledge the real risks involved. These include potential injury to the inferior alveolar nerve if planning is inadequate, creation of buccal or lingual fenestrations in the mandible (particularly in the sublingual fossa) and, in the maxilla - failure to recognize defects or cracks in the anterior region where guided bone regeneration may have been indicated but not performed. Bone volume assessment is central to all of this. In the sinus region, for example, I have personally experienced an implant dislodging into the sinus while attempting an indirect sinus lift. These are not rare or extraordinary complications; they are common things that can go wrong if implant dentistry is approached casually or without adequate preparation.
This is precisely why implantology must be approached with caution. It is not as simple as it is sometimes portrayed to be, nor is it as straightforward as certain narratives make it sound.
Dr. Akriti: How do you handle cases that require bone grafting or sinus lift? Do you prefer a staged approach or a single-stage procedure, and what factors guide your decision?
Dr. Darshan Parikh: Over time, our approach has naturally evolved based on exposure, training, and the protocols we have learned and tested. We have worked across the entire spectrum of implant workflows: extraction with socket grafting, immediate implant placement, immediate placement with contour augmentation, and socket preservation using techniques such as the ice-cream cone method to rebuild the site for delayed implant placement. We have performed indirect sinus lifts, staged direct sinus lifts, and, more recently, simultaneous sinus lift and implant placement. My training has played a decisive role here. With structured exposure through programs like IFZI, where sinus lift procedures are actively taught and practiced, it becomes possible to confidently perform a sinus lift and place the implant simultaneously. That said, the decision is never technique-driven; it is always case-driven. The fundamental question remains the same in every scenario: do you have enough residual bone to achieve primary stability? If the answer is yes, a simultaneous sinus lift and implant placement may be appropriate. If the residual bone is insufficient, then irrespective of having learned the technique, simultaneous placement should not be attempted. In such cases, grafting alone and allowing adequate healing is the correct and safer choice. Training expands capability, but it does not replace judgment.
Equally important is mental rehearsal and preparedness. Before taking the patient up for surgery, the plan must be reviewed multiple times. More importantly, the surgeon must be prepared to abandon the procedure if intraoperative findings do not match the plan. You may reflect the flap, begin the osteotomy, and realize within the first or second drill that there is simply inadequate bone to place an implant. In such situations, abandoning the implant placement is not failure; it is responsible clinical decision-making. It is always better to be safe than to be adventurous.
Unfortunately, when cases fail, there is a tendency to blame the graft material or the patient’s compliance. However, both rational thinking and robust research consistently show that one of the most critical determinants of implant success is the operator. The clinician’s knowledge base, surgical skill, planning ability, instrumentation, and material selection play a decisive role. This is why implant dentistry should never be approached with a “jugad” mindset. Using inferior grafts, compromised instruments, or shortcuts simply because they are cheaper is not acceptable. If one wishes to carry the professional identity of an implantologist, one must also uphold higher clinical and ethical standards. That includes gradually investing in appropriate systems, quality instruments, and reliable biomaterials, even if it takes time.
With that comes an important psychological shift. When you invest correctly, you also become comfortable charging appropriately. You no longer feel guilty about treatment costs because you understand the true value of what you are providing. Personally, my approach in the initial learning phase has been very clear. The first few times I perform a new procedure, I often do not charge the patient. I view it as paying to learn. If I place a graft worth ₹5,000–10,000, I consider that an investment in my education. If it fails, the patient has not suffered a financial loss. If it succeeds, I have gained experience, confidence, and clarity about the true cost of the procedure. After performing a few such cases, confidence builds, outcomes become predictable, and you develop a realistic understanding of expenses. At that point, you are in a position to price the procedure ethically and sustainably. This gradual, honest progression is what leads to long-term success in implant practice.
Dr. Akriti: Does the choice of surgical approach, such as flap versus flapless implant placement, influence the overall success of an implant? If so, how do you decide which approach is appropriate for a given case?
Dr. Darshan Parikh: Flapless surgery does have definite advantages from the patient’s perspective. Because you are not raising a flap, patients experience less postoperative pain, reduced swelling, and overall better comfort. Patient-reported outcomes, including visual analog scale scores, are consistently better with flapless approaches. However, and this is extremely important, flapless implant surgery should be performed only when it is fully guided surgery, and even then, only by experienced clinicians. Guided surgery is not for beginners. Unfortunately, what is happening today is that because CBCT centers and dental laboratories are readily offering surgical guides, a young dentist may feel that guided surgery makes implant placement easier or safer. That is the wrong way to approach implant dentistry. If you do not know what you are doing, if you cannot visualize the anatomy directly, and if you do not understand how to manage deviations or complications, guided surgery actually removes your ability to control the situation.
Guided surgery is a more advanced level of implant practice. While it offers many benefits like accuracy, reduced chair time, improved patient comfort, it also demands a high level of foundational surgical understanding. When you are starting out, you must learn how to raise a flap.
Flap elevation is not a single technique. There are multiple flap designs, each with specific indications and long-term implications. These include envelope flaps, papilla-preserving flaps, triangular flaps, and trapezoidal flaps. Choosing the correct flap design depends on the case, particularly from the perspective of soft-tissue management and long-term maintenance. Soft tissue plays a critical role in implant success. Therefore, flap design and suturing are extremely important skills.
While flapless surgery is perceived better by patients and is associated with reduced morbidity, it should be reserved for experienced clinicians who have already developed strong surgical judgment. In my opinion, you should have placed at least 50 to 80, ideally closer to 100 implants, before attempting flapless procedures independently. Even then, the same principles apply: you must thoroughly understand the implant system you are using, know the drill sequence, respect the manufacturer’s protocols, and be aware of the system’s limitations. Guided surgery does not compensate for lack of knowledge or experience.
Dr. Akriti: Do you perform guided implants or prefer the traditional method?
Dr. Darshan Parikh: We use both approaches, freehand as well as guided surgery. For relatively straightforward cases and even for full-arch rehabilitations in some situations, we perform what is often referred to as “brain-guided” surgery.
That said, guided surgery does offer definite advantages. In larger cases, in particular, the use of a surgical guide significantly simplifies the procedure and improves patient comfort. When you reflect a flap, place multiple implants, and then suture the site, the surgical time increases considerably. With guided surgery, the steps of flap reflection and suturing, often accounting for 15 to 30 minutes or more, can significantly reduced. This makes the procedure faster and less invasive for the patient. However, the decision to use guided surgery must always be case-dependent and based on proper planning. Another important factor is the cost and whether the patient can realistically afford it. A surgical guide comes at an additional expense, and this must be factored into the treatment plan. As per current costs, at least in Pune, a guide typically costs around ₹2,500 to ₹3,000 for a single guide and one implant. For multiple implants, the cost structure usually involves a base price for the guide, with an additional charge of approximately ₹1,000 per extra implant. For example, in a three-implant case, the total guide-related cost may be around ₹5,500. The critical question, then, is: who bears this cost? If the clinician has already priced it into the overall treatment fee, guided surgery becomes viable. If not, it directly impacts profitability. Therefore, financial planning is as important as surgical planning.
It is also essential to understand that guided surgery is not a universal solution or a “one-size-fits-all” approach. It is not a shortcut or a guaranteed remedy for every case. There are clear indications for guided surgery, and it should be used when those indications are present. That said, if you have a well-established digital workflow and the case allows for it, even situations that can be managed freehand may benefit from guided placement in terms of accuracy, efficiency, and patient experience.
This section highlights that implant success is not defined by technique alone, but by planning depth, surgical adaptability, ethical decision-making, and respect for biological principles; the skills that mature only with experience. The fifth part talks about a bigger question: what does success in implant dentistry really look like, years after the procedure is done?