Early Detection of Oral Cancer in India: Dr. Bhuvan Nagpal on Barriers, Blind Spots, and Solutions (Part-2)
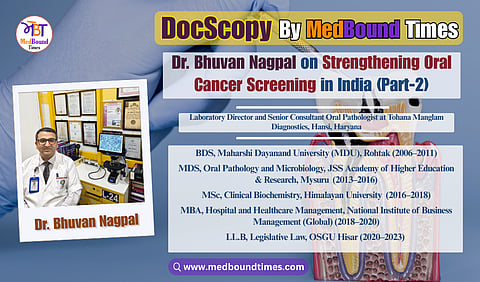
In an era where early diagnosis can mean the difference between timely intervention and advanced disease, oral pathology plays a quietly critical role in dentistry and cancer prevention. MedBound Times spoke with Dr. Bhuvan Nagpal, a distinguished oral and maxillofacial pathologist, clinical biochemist, and medico-legal consultant whose work spans diagnostics, research, public health, and healthcare law. With an extensive academic background that includes BDS (MDU, Rohtak), MDS (JSS, Mysuru), PGT in Head and Neck Oral Pathology, MSc, MBA, PGDMLS, LL.B, Ph.D (Honorary), and multiple professional certifications including CLQMS and FPFA (USA), Dr. Nagpal exemplifies lifelong learning and academic rigor, positioning himself at the intersection of precision diagnostics and multidisciplinary healthcare practice.
Currently serving as the Director of Tohana Manglam Diagnostics and a Business Partner at Manglam Diagnostics, Hansi, Haryana, Dr. Nagpal’s clinical focus lies in histopathological evaluation, early identification of oral potentially malignant disorders, and comprehensive head and neck diagnostics. Beyond clinical practice, he is the Founder and President of the Practicing Oral Pathologists and Microbiologists Association (POPMA) and the driving force behind the Centre for Oral Pathology and Maxillofacial Diagnostics (COPMD), India’s first dedicated chain of oral pathology diagnostic centres, aimed at strengthening the visibility and impact of oral pathology nationwide.
In this DocScopy interview, conducted by Dr. Akriti Mishra, Dr. Nagpal highlights the challenges of early oral cancer detection in India, including gaps in awareness, delayed reporting, social stigma, and limited screening access.
Dr. Akriti : What are the main barriers (social, cultural, infrastructural) that prevent early diagnosis and screening of oral cancer in India?
Dr. Bhuvan Nagpal : Unfortunately, several interlinked barriers hinder early diagnosis and timely screening of oral cancer in India, many of which stem from gaps in awareness, accessibility, and healthcare delivery.
Low Public Awareness: One of the most significant challenges is that a vast segment of the population is simply unaware of the early signs of oral cancer or the importance of routine screening. Research consistently shows that over 80% of patients are not informed about their personal risk, and more than 83% don’t know that early detection is possible through a simple mouth exam. Many only seek medical help when symptoms become painful or visibly advanced, often too late for conservative treatment.
Cultural and Social Norms: Tobacco chewing (gutkha, pan masala), betel quid, and areca nut use are socially ingrained practices in many communities. These are known carcinogens yet they remain culturally accepted, even among women, especially in rural areas where smokeless tobacco is perceived as harmless. Misconceptions also persist, with many attributing persistent ulcers or patches to “body heat” or minor irritation. Additionally, fear and stigma surrounding cancer, seen as a death sentence or source of social shame, discourage people from seeking early evaluation.
Infrastructural Gaps and Accessibility Issues: India's healthcare infrastructure, particularly in rural and remote areas, is not yet equipped to support widespread oral cancer screening. Less than 1% of the population has undergone oral screening in recent years. Many at-risk individuals lack access to diagnostic centers or oral pathology services. Distance to hospitals, travel costs, loss of daily wages, and lack of family support often delay follow-ups, even when free camps are organized.
Gaps Within the Healthcare System: Many general practitioners and even dental professionals may not be fully trained to detect early signs of oral cancer or may not perform routine mucosal screenings. Even though national programs such as the National Tobacco Control Program and oral cancer screening initiatives exist on paper, ground-level implementation remains inconsistent due to logistical challenges, funding gaps, and limited outreach.
In summary, the barriers are multifaceted, including a blend of low awareness, cultural habits, social stigma, limited access to diagnostic facilities, and underutilization of screening programs. Overcoming them will require a comprehensive strategy: community education, integration of screening into routine primary care, training healthcare providers, and improving accessibility through mobile units, rural clinics, and subsidized services. Making early detection both familiar and feasible is the key to turning the tide against India’s oral cancer epidemic.
Dr. Akriti : Why is early detection of oral cancer so critical and what are the most common “silent signs” patients or dentists should watch for?
Dr. Bhuvan Nagpal : Early detection of oral cancer is critical because it truly saves lives and preserves quality of life. The difference in outcomes is striking: when detected at an early stage, the 5-year survival rate is approximately 80–84%. In contrast, if the cancer is diagnosed late, after it has spread to lymph nodes or deeper tissues, survival drops dramatically to 30–40%. Early-stage cancers are generally smaller and haven’t spread to lymph nodes, thus more responsive to treatment. The patient can often avoid the disfiguring surgeries or aggressive treatments that advanced cancers require. In short, early detection makes the cancer far more treatable, with a higher chance of cure and lower treatment-related morbidity. It’s not just about living longer, but also about retaining the ability to speak, chew, and swallow normally. So, from a medical and a quality-of-life standpoint, early detection is paramount.
The challenge is that oral cancer often begins with “silent signs” and symptoms that are painless, subtle, or easily overlooked. These include:
Persistent ulcers or sores in the mouth that don’t heal within two weeks
White patches (leukoplakia) on the gums, tongue, or cheeks that can’t be scraped off - some harbor early cancerous changes
Red or red-white patches (erythroplakia), which have an even higher risk of malignant transformation
Lumps or thickened areas in the lining of the mouth, tongue, or jaw
Unexplained numbness, tingling, or bleeding in the mouth
Loosening of teeth or poor denture fit without dental cause
Chronic sore throat, hoarseness, or difficulty in swallowing
These signs are often painless, which is why patients may ignore them. A painless ulcer or a small red patch may not seem alarming, but these can be the earliest indicators of something more serious.
The key point I tell patients and dentists is: anything that is unusual and lasting more than 10-14 days should be checked. Early lesions typically don’t hurt. Cancer may start as a tiny painless ulcer or patch. Because they’re “silent,” these signs often get overlooked or attributed to minor causes. We need to educate everyone that these subtle changes (a persistent ulcer, an odd-colored patch, an unexplained lump) are exactly the signs to watch for. Recognizing them and getting them evaluated promptly (with a biopsy) is the best way to catch oral cancer at an early, curable stage.
Awareness and vigilance are the keys to prevention.
Dr. Akriti : In your view, how effective are self-examinations and routine dental screenings in catching pre-cancerous or malignant lesions early in India?
Dr. Bhuvan Nagpal : Both self-examinations and routine dental screenings can be very effective tools for early detection – but currently in India they are under-utilized, which limits their impact. Let’s break it down:
Self-examinations: An oral self-exam is basically when a person checks their own mouth regularly (say once a month) using a mirror and good lighting, looking for any of the “silent signs” we just discussed. In theory, this is a simple, inexpensive, and empowering strategy for early detection. If people examine themselves, they might notice a new patch or ulcer and seek care sooner. However, the reality in India right now is that awareness of oral self-examination is extremely low. One recent study among oral cancer patients found literally 0% of them were aware of self-examination – none had ever been taught or told to do it. So, while I strongly encourage people to perform self-exams (I often teach patients how to do it during awareness camps, telling them to use their fingers and mirror to check all around the mouth), its effectiveness is limited by the fact that most people don’t know about it or remember to do it. In urban, educated populations that follow health information, self-exams could catch things early – for example, someone might feel a small lump or see a red patch and go to the dentist. We need more public health campaigns to teach self-exam techniques (much like breast self-exam campaigns) to make this a widespread practice. In summary, self-exams are potentially very effective, but in practice here, we have a long way to go in making them common.
Routine dental screenings: This refers to dentists performing an oral cancer screening on every patient as part of a regular dental check-up (or through special screening camps). In my opinion, this is one of the most effective ways to catch lesions early – if it’s actually done routinely. Dentists are in a prime position because they see patients who may not have any symptoms yet, and a quick 5-minute examination of the mouth can reveal early abnormalities. In countries where dentistry is more preventive, dentists have indeed caught many oral cancers at an early stage simply by doing an annual exam. In India, however, the challenge is twofold: not enough people visit the dentist regularly, and not all dentists systematically screen for oral cancer on every visit. Many individuals here only go to a dentist when they have pain or a major tooth problem, and even during those visits, the focus might stay on the immediate complaint (like a toothache) unless the dentist makes a conscious effort to do a full oral mucosal check.
That said, when routine screenings are implemented, they make a big difference. We have seen in community dental camps and government initiatives that if you screen a large at-risk population, you will definitely find a number of leukoplakias, early cancers, etc., that the people were completely unaware of. Research from public health experts has concluded that conducting frequent cancer awareness and screening camps will detect oral cancers at an early stage in more people. The effectiveness is proven by those findings – early-stage detection goes up with regular screening. The issue is scaling it up. As I mentioned earlier, the National Family Health Survey-5 reported that less than 1% of the Indian population had ever undergone an oral cancer screening exam in a two-year period, which is shockingly low. This means 99% of people are not getting examined and any precancerous lesions they have might quietly progress.
In my practice, whenever we do a screening event or when a patient comes in for, say, a routine cleaning, we make it a point to do a thorough oral exam. We have indeed caught precancerous lesions like erythroplakia or early-stage cancers in people who had no idea these existed – and we referred them for timely treatment. The effectiveness, in those cases, is clear: a life potentially saved because of a routine check.
To summarise, both self-examinations and routine screenings are powerful tools, but their effectiveness depends on widespread awareness and consistent implementation. Encouraging the public to self-examine and equipping dentists to screen every patient routinely can drastically increase early detection and improve survival outcomes across India.
In this section, Dr. Bhuvan Nagpal discusses the barriers that hinder early oral cancer detection in India, highlighting how gaps in awareness, delayed presentation, social stigma, and limited screening contribute to late-stage diagnosis. He emphasizes why addressing these challenges is critical to improving outcomes at a population level. In Part 3, Dr. Nagpal shifts focus to the clinical side of prevention, discussing key risk factors, diagnostic aids, and preventive strategies that enable timely and accurate identification of oral cancer, ultimately helping reduce its overall burden.