Scientists at La Jolla Institute for Immunology (LJI) have published an in-depth study into how the immune system’s T cells target pediatric brain tumors. Their research suggests that a small number of pediatric brain tumor patients already have cancer-fighting T cells within their tumors.
This discovery, published recently in Nature Cancer, is an important step toward helping identify which pediatric brain tumor patients might benefit from cancer-fighting immunotherapies.
“These patients may be candidates in whom immunotherapy has the potential to show clinical benefit,” LJI Clinical Associate and UC San Diego Assistant Professor Anusha Preethi Ganesan, M.D., Ph.D., who co-led the new study with LJI Professor Pandurangan Vijayanand, M.D., Ph.D. “Future clinical trials that test immunotherapy in such selected patients are required to verify these findings.”
Immunotherapies prompt a patient’s own immune cells to destroy cancer cells. For an immunotherapy to work, T cells need to “see” the tell-tale mutations—the genetic red flags—that separate tumor cells from normal cells. One type of immunotherapy, called immune checkpoint blockade, makes it easier for T cells to detect and destroy tumors and has proven effective for many types of adult cancers.
Unfortunately, clinical trials for immunotherapies in pediatric patients have shown inconsistent results, and no immunotherapy has been approved yet for use in children.
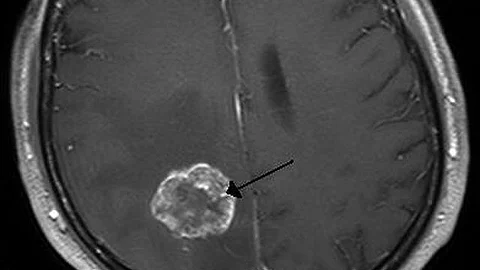
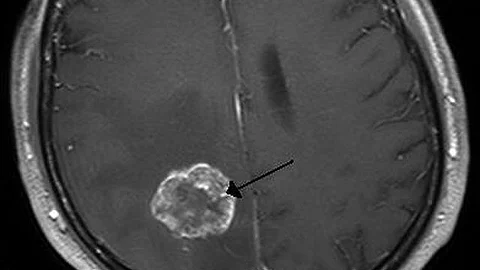
This failure has led some to wonder if T cells can even detect pediatric brain tumors. Perhaps these brain tumor cells don’t have enough genetic mutations to trigger a strong T cell response? “The notion that brain tumors are ‘immune cold’ with low mutation burden precluded the assessment of T cell responses in children,” says Ganesan, who is also a practicing pediatric oncologist at Rady Children’s Hospital.
For the new study, Ganesan collected tumor samples from 38 children who had been patients at Rady Children’s Hospital in San Diego. The team looked for T cells within the tumors, and discovered that T cell levels varied widely between patients. This variation may help explain why immunotherapy trials in children have shown such inconsistent results.
LJI Postdoctoral Researcher Aditi Upadhye, Ph.D., says it is encouraging to find T cells in even a small number of pediatric tumors. “No one had really known if there were even T cells in these tumors,” says Upadhye, who served as study co-first author with LJI LJI Bioinformatic Scientist Kevin Meza Landeros.
The researchers then used genetic sequencing tools to examine more than 41,000 T cells found in these brain tumor samples. They looked at gene expression in these T cells to see whether the cells could potentially destroy tumors.
They found that a small number of patients had large numbers of T cells that responded to markers, called neoantigens, on the brain tumor cells. These T cells appeared to have “effector” functions, which means they could potentially destroy tumor cells. “T cells are infiltrating the brain, and they may be possibly responding to tumor cells,” says Meza Landeros.
The researchers are now working to translate these findings to the clinic. They hope to learn exactly which neoantigens prompt the strongest T cell responses. In the end, they hope to help doctors identify which pediatric patients might benefit from immunotherapies, such as immune checkpoint blockade.
These findings need to be validated in clinical trials,” says Vijayanand, a member of the LJI Center for Cancer Immunotherapy. “But this study gives us cautious optimism.”
The scientists emphasized the importance of philanthropic support for this research. The research received significant funding through Curebound, Hyundai Hope on Wheels, and the Peacock Foundation. Ganesan has received ongoing support from Curebound to follow up on the brain tumor data from this study. “I am grateful for the funding and support from these groups,” says Ganesan.
“That funding made a difference,” adds Vijayanand. “The donors and foundations that supported this work are very appreciated.”
Additional authors of the study, “Intra-tumoral T cells in pediatric brain tumors display clonal expansion and effector properties,” include Ciro Ramírez-Suástegui, Benjamin J. Schmiedel, Edwin Woo, Serena J. Chee, Denise Malicki, Nicole G. Coufal, David Gonda, Michael L. Levy, Jason A. Greenbaum, Grégory Seumois, John Crawford, William D. Roberts, Stephen P. Schoenberger, Hilde Cheroutre, and Christian H. Ottensmeier.
This research was
This research was also supported by the Whitaker Fund, William K. Bowes Jr Foundation, and the National Institutes of Health (K08 CA230164).
DOI: https://doi.org/10.1038/s43018-023-00706-9
About La Jolla Institute
La Jolla Institute for Immunology is dedicated to understanding the intricacies and power of the immune system so that we may apply that knowledge to promote human health and prevent a wide range of diseases. Since its founding in 1988 as an independent, nonprofit research organization, the Institute has made numerous advances leading toward its goal: life without disease. Visit lji.org for more information.
(KB/Newswise)
