In a scientific breakthrough, Mount Sinai researchers have revealed the biological mechanisms by which a family of proteins known as histone deacetylases (HDACs) activate immune system cells linked to inflammatory bowel disease (IBD) and other inflammatory diseases.
This discovery, reported in Proceedings of the National Academy of Sciences (PNAS), could potentially lead to the development of selective HDAC inhibitors designed to treat types of IBD such as ulcerative colitis and Crohn’s disease.
“Our understanding of the specific function of class II HDACs in different cell types has been limited, impeding development of therapies targeting this promising drug target family,” says senior author Ming-Ming Zhou, PhD, Dr. Harold and Golden Lamport Professor in Physiology and Biophysics and Chair of the Department of Pharmacological Sciences at the Icahn School of Medicine at Mount Sinai. “Through our proof-of-concept study, we’re unraveling the mechanisms of class II HDACs, providing essential knowledge to explore their therapeutic potential for safer and more effective disease treatments.”
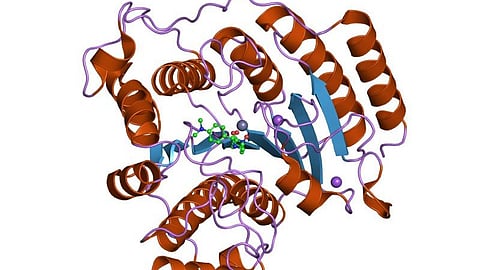
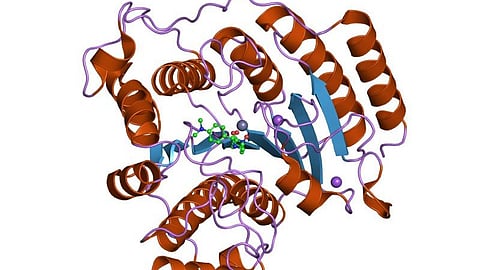
The Mount Sinai team focused specifically on class IIa HDACs, which exhibit more tissue-specific functions than class I HDACs, which act more broadly. Among the 18 histone deacetylases discovered to date in mammals, HDAC4 and HDAC7—both class IIa HDACs—stand out for their roles in regulating the development and differentiation of Th17 cells. These cells are known for producing interleukin-17 (IL-17), a highly inflammatory cytokine associated with a spectrum of disorders, including IBD, multiple sclerosis, and rheumatoid arthritis. Given the strong correlation between excessive Th17 cell activity and human disease, scientists have focused on pharmacological or genetic interventions targeting HDAC4/7 to mitigate Th17 cell-mediated inflammation.
In their groundbreaking study, the Mount Sinai researchers delineated a previously unrecognized mechanism by which HDAC4 and HDAC7 operate independently yet cooperatively to govern Th17 cell differentiation and transcription. Transcription is the initial step of gene expression involving copying of the DNA sequence to generate RNA molecules; it is crucial for most biological processes.
“The role of class IIa HDACs in Th17 cells and inflammatory disease has been largely unexplored until now,” notes lead author Ka Lung Cheung, PhD, Assistant Professor of Pharmacological Sciences at Icahn Mount Sinai. “Mechanistically, we’ve discovered that class IIa HDACs orchestrate both gene transcriptional activation and repression to steer the process of Th17 cell differentiation. This significant revelation deepens our comprehension of the previously ambiguous role of class IIa HDACs in biology and human disease.”
As a critical aspect of their investigation, the research team found that a potent class IIa HDAC inhibitor, TMP269, influenced the differentiation of Th17 cells in a mouse model of ulcerative colitis. This pivotal discovery underscored the potential of pharmacological inhibition of class IIa HDACs as a promising therapeutic approach for addressing Th17-related inflammatory and autoimmune diseases, the study reported.
Expanding on this foundation of knowledge, researchers in the Zhou Lab and the Cheung Lab at Mount Sinai plan to concentrate on refining class IIa HDAC inhibitors with better efficacies for treating various types of Th17-mediated diseases.
“While our study primarily examined inflammatory bowel disease, specifically colitis,” says Dr. Zhou, “we believe our findings pave the way for extensive research into advanced therapies targeting severe inflammation in various other pathologies within the human body.”
(Newswise/KV)
