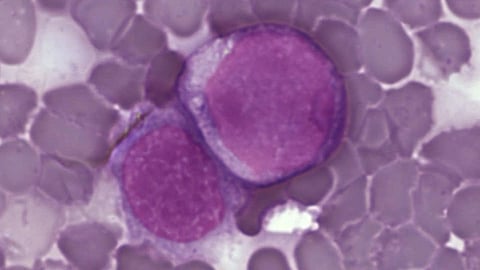
Acute myeloid leukemia (AML) is an aggressive form of cancer that originates in the bone marrow, rapidly spreads to the blood and can quickly cause death if not treated promptly. Despite recent therapeutic advances, it continues to be associated with poor outcomes in the majority of patients with this disease.
New research from VCU Massey Cancer Center suggests that a novel type of combination therapy could offer key insights into future treatment strategies for AML patients.
Venetoclax is an oral medication that binds to and blocks the function of a cancer-driving protein called BCL2, and thereby helps to kill AML cells, while rendering them more sensitive to other anti-cancer agents. Venetoclax has been approved for the treatment of certain patients with AML when combined with another anti-leukemic agent (5-azacytidine). Unfortunately, AML cells often develop resistance to venetoclax, highlighting the need for new therapeutic strategies designed to overcome this problem.
Through a study recently published in Clinical Cancer Research — the translational journal of the American Association for Cancer Research — Steven Grant, M.D., associate director for translational research and co-leader of the Developmental Therapeutics research program at Massey, along with his collaborators determined that using a class of drugs known as dual mTORC1/2 inhibitors in combination with venetoclax dramatically suppressed the growth of a variety of human leukemic cell types, including cells taken from AML patients.
Dual mTORC1/2 inhibitors disrupt downstream components of a cascade known as the AKT pathway which is frequently deregulated in many forms of cancer, including AML.
“This combination substantially triggered AML cell death, including those resistant to venetoclax through both intrinsic as well as acquired mechanisms,” said Grant, who is also the Shirley Carter and Sture Gordon Olsson Chair in Cancer Research at Massey, as well as a professor and eminent scholar in the Department of Internal Medicine at the VCU School of Medicine.
Notably, the combination of venetoclax with dual mTORC1/2 inhibitors was more effective against AML cells with a highly active AKT genetic pathway compared to combinations with other inhibitors of this same pathway (e.g. PI3 kinase or AKT antagonists).
“Our findings raise the possibility that pairing a dual mTORC1/2 inhibitor with venetoclax may represent a new and potentially effective treatment option for patients with AML,” Grant said.
In pre-clinical studies, the research team observed that the drug combination successfully killed AML cells, but an identical regimen was significantly less toxic to normal blood cells, raising the possibility of therapeutic selectivity. The combination was effective in several mouse models of AML, including those involving patient-derived xenografts (PDX) models.
Grant believes these findings also raise the possibility that this therapeutic combination could be particularly effective against leukemia cells in which the AKT pathway may be highly active. Prospective studies designed to test this hypothesis are currently underway.
“Our findings may represent the first steps toward a potentially promising addition to the therapeutic armamentarium for AML,” Grant said.(GN/Newswise)
